Chronic kidney disease affects one in seven people in our country.
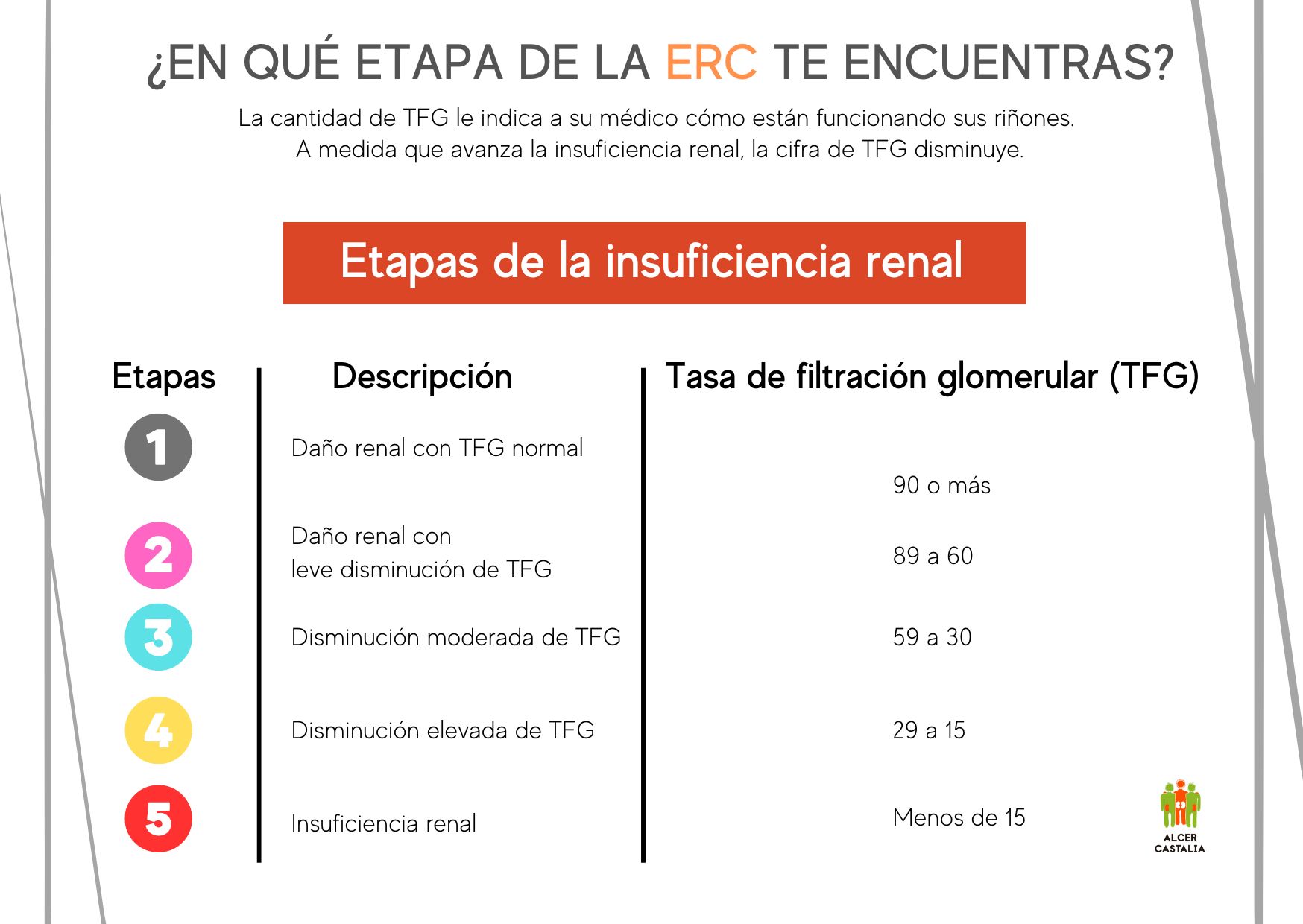
Chronic kidney disease (CKD) is a condition characterized by a significant and progressive decrease in kidney function. CKD is defined as a decrease in kidney function, expressed by an estimated glomerular filtration rate (GFR) or creatinine clearance < 60 ml/min/1.73 m2, or as the presence of persistent kidney damage for at least 3 months.
Kidney damage is usually diagnosed using markers, the main marker of kidney damage is elevated urinary albumin or protein excretion. Within CKD there are various stages that stratify the level of progression of the disease.
Kidney diseases, in general, are known as nephropathies and have a variable evolution:
- Sometimes kidney function is affected quickly, other times little by little.
- Sometimes, there is no cure and the damage continues its course, and in others, the disease is stopped and part, or practically all, of the function of the organs is recovered.
In any of the cases in which the kidney disease is unstoppable, or the injury is very important, the part that remains in operation will decrease and its cleaning work will be insufficient, although the person does not notice it as they are asymptomatic, or have symptoms that are not related to loss of kidney function.
Stages 3-5 constitute what is commonly known as Chronic Kidney Failure (CKD). Advanced Chronic Kidney Disease (ACKD) includes stages 4 and 5. Chronic kidney disease is therefore defined as one that causes a severe decrease in glomerular filtration (GFR < 30 ml/min). ). Therapeutic objectives are aimed at reducing and treating the complications associated with kidney failure, and preparing adequately, and with sufficient advance notice, the replacement treatment since due to this lack of kidney function (among other consequences, it decreases the quantity and quality of urine) substances not eliminated in the urine will accumulate in the body.
This pathology may not cause pain or discomfort, and in many cases there will be no feeling of illness, even if a large part of kidney function has been lost. However, follow-up work in nephrology consultations can greatly delay the progression of the disease, even stopping it in some processes if action is taken at the beginning.
It is very important that the person who suffers from these problems knows about them and collaborates with the professionals in charge of their care. During this follow-up period, the nephrology consultation will control all the risk factors that can be modified, the diseases that may appear, the medications that impair kidney function, the foods that are recommended and those that are not, etc.
Symptoms
Some of the symptoms that may appear when kidney function decreases are:
- The kidneys will stop making urine and if they make it, it will become increasingly clearer since the toxic substances will not be eliminated from our body (they remain in the blood).
- Accumulation of fluids and waste in the body, which will cause general discomfort.
- Increased nighttime urination.
- Feeling of tiredness and, in cases of also having anemia, pale skin color.
- Lack of appetite and sometimes nausea and vomiting.
- High blood pressure.
- You may have a fever without another cause.
If CKD progresses, more symptoms may appear such as:
- Itchy skin.
- Tingling and cramps, especially in the legs.
- Bone pain.
- Bad breath.
- Straw heat of the skin.
However, we must not forget that, sometimes, the decrease in kidney function is not accompanied by symptoms until very advanced stages of the disease, which is why it is said to be a silent disease, but this does not mean that CKD is not present and does not progress.
Treatment
Those people in an advanced stage of the disease require treatment that compensates for the main functions of the kidneys since, when they do not work, or do not work well, many toxins and liquid that are harmful to their body accumulate.< /p>
Currently, there are five types of kidney replacement treatments:
- Hemodialysis – is a procedure by which blood, through a system of tubes, reaches the artificial kidney (machine), passes through a special filter and is returned to the body. The patient must travel to the dialysis center every two days to receive the treatment.
- Home hemodialysis – is the same procedure as hemodialysis, but is performed in the affected person’s home. To do this, hospital training will be carried out to learn how the dialyzing machine works and the appropriate way to puncture or, where appropriate, connect to the catheter.
- Peritoneal dialysis – is a technique in which the blood is cleaned inside the abdomen of the person with CKD, which acts as a filter. It has the advantage of time flexibility, just like home hemodialysis. It is a technique that is performed throughout the day.
- Peritoneal dialysis with a cycler – the technique is the same as peritoneal dialysis, the only thing that is done at night and automatically through the cycler, in charge of making the replacements. li>
- Kidney transplant – the transplant consists of implanting a kidney into a person whose kidneys do not work. When it is possible to do so, it is the most desirable solution because:
- It allows the person to free themselves from dependence on a machine.
- The symptoms of the disease and the limitations that dialysis implies disappear, with a great improvement in the quality of life of the transplanted person.
The kidney that is transplanted comes from:
- A living donor, where the characteristics of the donor and the recipient must be compatible to avoid rejection. Normally, they are people related to each other.
- A deceased donor, who during life has donated his or her organs so that they can save other lives.
Thousands of lives are lost every year because there are not enough organ donors. An organ, if successfully transplanted, is literally a gift of life.
Prevention
Once all this has been explained, we can say that one of the objectives of our entity is to prevent more people from being diagnosed with CKD, that is, to start at the beginning to save ourselves the entire path explained previously.
We know that there are diseases that cannot be avoided, but in many cases, we can do our part to positively influence our body.
Here we leave you several ideas to do it:
- Control glucose
- Avoid stress
- Avoid smoking
- Go to the doctor if you have urinary discomfort, alterations or bad appearance of your urine
- Control blood pressure
- Eat a diet rich in vegetables and legumes, and low in saturated fats
- Avoid excess weight
- Always take medication under medical supervision
- Avoid alcohol consumption
- Do physical activity regularly
- Cook your food boiled or grilled
- Decrease salt consumption
- Complies with the treatment for infectious processes
For more information we invite you to go to this section.
Where are we?
ALCER Castalia has its headquarters in a central office building, on Enmedio Street, 22 in the city of Castelló de la Plana.
Due to the expansion of services, we are distributed in three offices, from where, in addition to management and coordination, we carry out part of the care, as well as various activities.
Currently, the distribution of the three offices is as follows:
- ALCER 4A Offices - A main office, where management and administration, social care, nutritional care and coordination of activities are located.
- Offices Transport: 4F - An office with two offices: transportation management and psychological care.
- Room multifunctional 2nd E - An office with a large room for holding meetings and activities (workshops, talks...), a warehouse and an office for service.